Starting the Conversation: A Resource for Health Care and Social Service Professionals on Social Isolation and Loneliness in Older Adults
Social isolation and loneliness are both potential issues that may negatively affect the mental and physical health of older adults — but they are not an inevitable part of aging. Health care and social service professionals (HCSSPs) are in a unique position to recognize the signs and help initiate meaningful conversations to support the social health of older adult patients or clients.
Why It Matters
In Canada, up to 41% of adults aged 50 and older are at risk of social isolation, and as many as 58% report experiencing loneliness. These issues are more than just emotional—they are linked to serious health outcomes, including:
- A 32% increased risk of stroke
- A 25% increased risk of cancer-related death
- A 50% increased risk of developing dementia
- A 45% increased risk of early mortality
Understanding the Difference
Although often linked, Social Isolation and Loneliness are distinct:
- Social isolation refers to having few social connections or interactions.
- Loneliness is the subjective feeling of being alone, regardless of actual social contact.
Not all time spent alone is negative on health.
Solitude can offer patients / clients valuable time for reflection, self-care and relaxation which are essential for mental and emotional well-being. However, finding a balance between solitude and social connection is key. This resource will help start supportive, respectful conversations that can lead to meaningful improvement.
About This Resource
This resource is designed to support HCSSPs in initiating open, compassionate conversations with older adults about social isolation and loneliness. These conversations aim to build trust and explore each patient’s /client’s unique experiences and strengths.
Because of the stigma that can sometimes be associated with loneliness, some clients or patients may not feel comfortable using that language or identifying with the term. Similarly, individuals who are socially isolated may feel content and connected in their own way.
Recognizing that every older adult’s situation is different, and the experiences of social isolation and loneliness is part of every person’s life journey, this resource encourages a personalized, non-judgmental approach based on the patient’s / client’s responses and needs.
It is important for professionals to understand the risk factors associated with social isolation
and loneliness, enabling them to recognize at-risk individuals and anticipate life changes that
may increase vulnerability.
Screening for social isolation and loneliness is essential for HCSSPs to identify older adults who
may be at risk, as these issues can significantly affect both physical and mental health. The use
of screening tools provides a consistent, evidence-based method for assessing risk and
informing appropriate interventions.
Checklist: Possible Indicators of Loneliness or Social Isolation
Discuss with your patient /client any of the potential changes or behaviours, which may suggest
a need for further assessment or supportive conversation:
Social Interaction
- Limited or no contact with family, friends, or community
- Noticeable withdrawal from usual social activities or routines
Emotional Wellbeing
- Expresses ongoing feelings of sadness or low mood
- Appears emotionally withdrawn or disinterested in conversation
Personal Care
- Decline in personal hygiene or grooming
- Neglect of household tasks or daily responsibilities
Physical Health & Complaints
- Frequent complaints of fatigue
- Regular reports of headaches or physical discomfort
- Sleep disturbances (e.g., trouble falling or staying asleep, oversleeping)
Did you Know?
To learn about available programs in your community, call 211 or visit 211.ca. Canada 211 is a free, confidential service available 24/7 that connects people to community and government resources in over 150 languages.
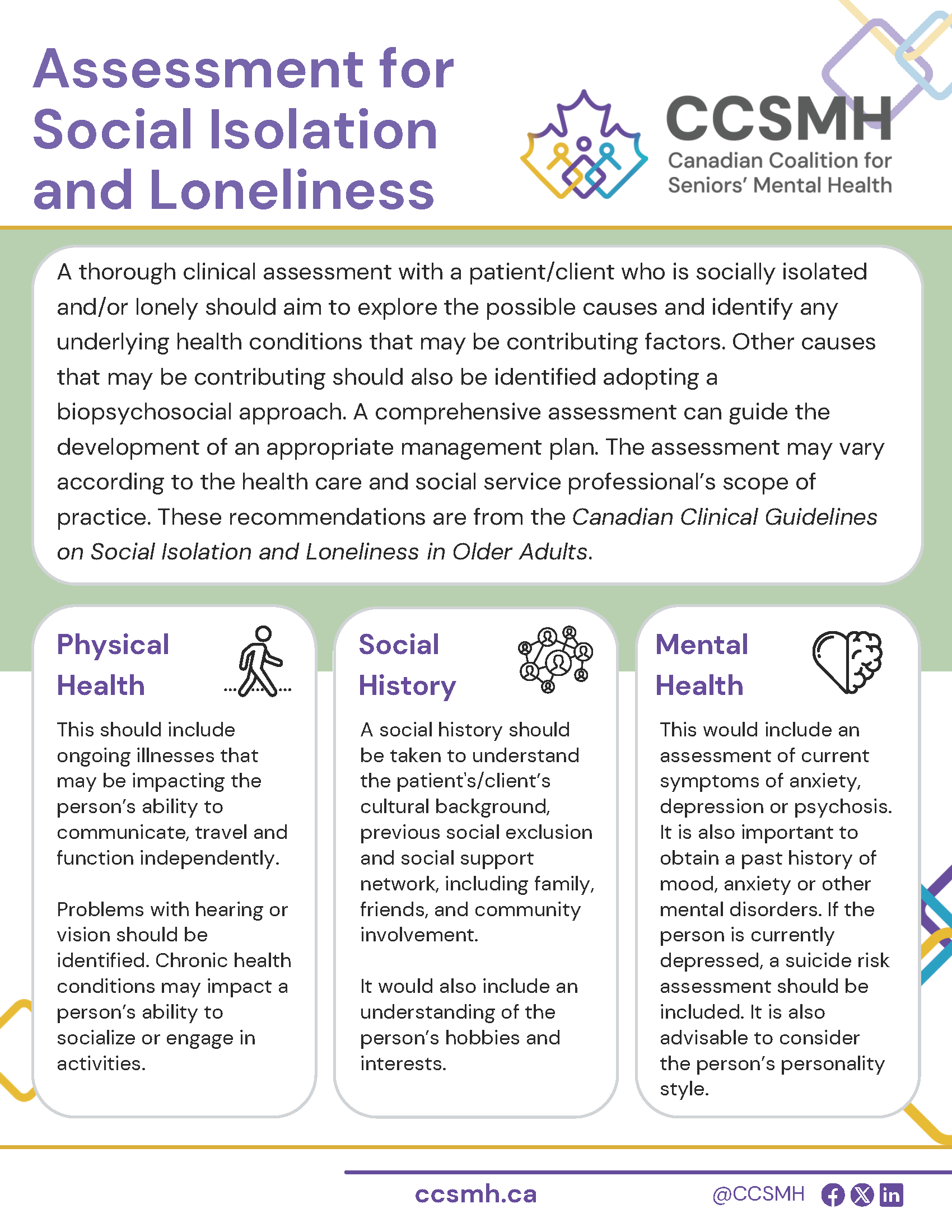
Learn More About the assessment of Social Isolation and Loneliness in Older Adults
A comprehensive assessment can guide the development of an appropriate management plan. Drawn from the guidelines, this resource is a helpful at-a-glance information sheet about the process of evaluating, assessing and treating social isolation and loneliness.
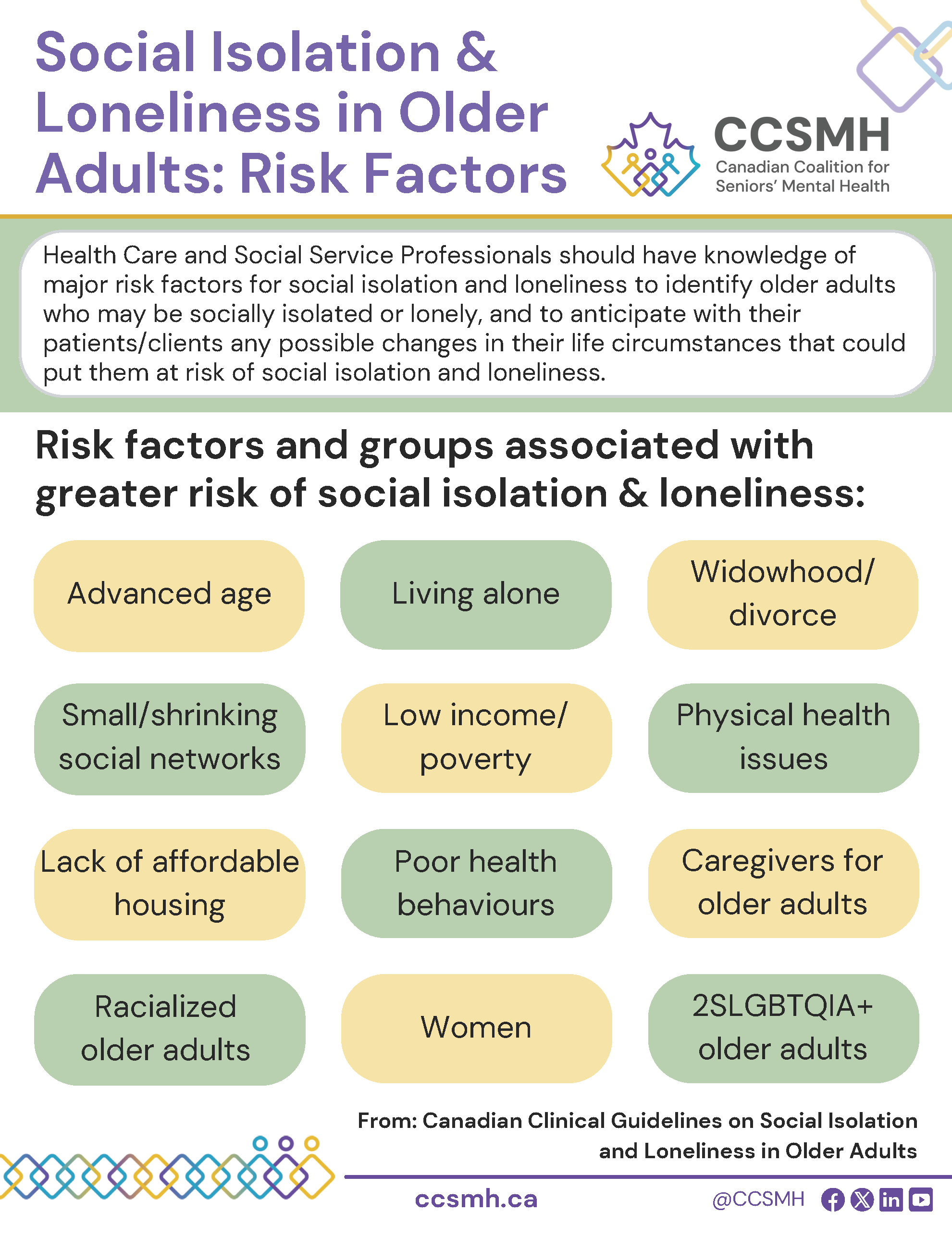
Learn More About Risk Factors
Health care and social service professionals should have knowledge of major risk factors for social isolation and loneliness to identify older adults who may be socially isolated or lonely. Drawn from the guidelines, this infographic is a helpful at-a-glance information sheet about the risk factors and groups associated with a greater risk of social isolation and loneliness.
Discover Key Takeaways From the Guidelines
Want to know more about key recommendations from the clinical guidelines? Print this infosheet for an at-a-glance reminder in your office and share it with your colleagues.
Clinical Guidelines
Discover the first guidelines on social isolation and loneliness in older adults.
For Health Care Professionals
Find clinical tools and resources to support your patients or clients.
Key Findings
Discover our research.
